Bugs that can infect the airways
Staphylococcus aureus
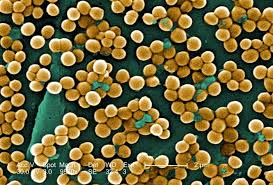 The Staph (pronounced 'staff') bacterium is a common cause of airway infection in young children. The regular twice daily flucloxacillin antibiotic that all children take for the first 2 years of life is used to try and reduce infection from this bug. It is treated with flucloxacillin, fuscidic acid or co-amoxyclav. For children on regular flucloxacillin, this is continued (taken 3 or 4 times per day) and a second antibiotic should be added. The Staph (pronounced 'staff') bacterium is a common cause of airway infection in young children. The regular twice daily flucloxacillin antibiotic that all children take for the first 2 years of life is used to try and reduce infection from this bug. It is treated with flucloxacillin, fuscidic acid or co-amoxyclav. For children on regular flucloxacillin, this is continued (taken 3 or 4 times per day) and a second antibiotic should be added.
Haemophilus influenzae
H-flu bacterial airway infection is common. Despite its name, it has nothing to do with 'flu that people get in the winter. It is usually easy to treat with either co-amoxyclav or cefaclor.
Pseudomonas aeruginosa
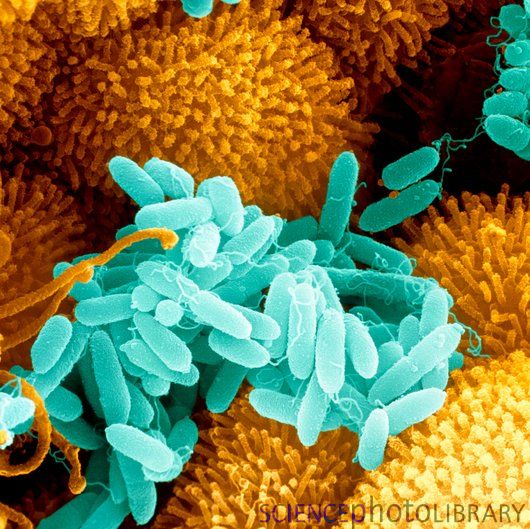 Pseudomonas (pronounced 'su-doh-moan-as') is a more troublesome infection. The Pseudomonas bug can be found in stagnant water (such as in U-bend of sinks), in soil and in rotting vegetation. Pseudomonas has 2 forms called 'mucoid' and 'non-mucoid'. When Pseudomonas first infects the airways, it is as the non-mucoid form, and when it is in this form it can be killed and the infection cleared. Once Pseudomonas has been in lungs for a few weeks it can change to the mucoid form. This means it covers itself with a protective coat of jelly, which makes it almost impossible to completely kill. When this has happened the airways are said to have 'chronic' (meaning long term) Pseudomonas infection. The strict definition of chronic infection is having 3 or more Pseudomonas positive airway cultures in a 12 month period. Studies have shown that lung function tends to be less good and get worse quicker when there is chronic Pseudomonas infection. Pseudomonas (pronounced 'su-doh-moan-as') is a more troublesome infection. The Pseudomonas bug can be found in stagnant water (such as in U-bend of sinks), in soil and in rotting vegetation. Pseudomonas has 2 forms called 'mucoid' and 'non-mucoid'. When Pseudomonas first infects the airways, it is as the non-mucoid form, and when it is in this form it can be killed and the infection cleared. Once Pseudomonas has been in lungs for a few weeks it can change to the mucoid form. This means it covers itself with a protective coat of jelly, which makes it almost impossible to completely kill. When this has happened the airways are said to have 'chronic' (meaning long term) Pseudomonas infection. The strict definition of chronic infection is having 3 or more Pseudomonas positive airway cultures in a 12 month period. Studies have shown that lung function tends to be less good and get worse quicker when there is chronic Pseudomonas infection.
Having said all that, Pseudomonas infection is quite common – about half of all children will have had at least one infection by the time they are 2 years old. If we find it and treat it early, there is a very good (better than 90%) chance it will go away. This is one of the main reasons for doing regular cough swabs and sputum samples.
What can be done to prevent Pseudomonas infection?
Sadly the answer is not much. We do recommend avoiding environments where Pseudomonas is likely to be present - such as stagnant water, home hot tubs or jacuzzis and home fish tanks. It is probably not a good idea to swim in lakes. Commercial pools are fine, as is swimming in the sea. Pseudomonas can also be present in rotting vegetation. In the home, Pseudomonas can be present in the u-bends of sinks - this is why sputum should not be disposed of down the sink - use the bin or the lavatory.
How is Pseudomonas treated?
There is only one oral antibiotic which works against Pseudomonas and that is ciprofloxacin. Ciprofloxacin used on its own is not very effective – it needs to be combined with an inhaled (nebulised) antibiotic. The first-line inhaled antibiotic we use is colomycin. By inhaling the antibiotic very high concentrations of antibiotic get into the mucous and kill the Pseudomonas bacteria. To try and make sure all the Pseudomonas are killed, the ciprofloxacin and the inhaled colomycin are both taken for 3 months.
An alternative approach is to use intravenous antibiotics combined with inhaled colomycin. The intravenous antibiotics are given for 2 weeks, and the colomycin is given for 3 months. No-one knows whether this works better, but it is more difficult and more stressful for the child and family, so at the moment we only use intravenous antibiotics if children who have grown Pseudomonas are unwell with a cough.
After 3 months treatment we will check to see if the Pseudomonas has gone (with repeat cough swabs or sputum samples). If it hasn't gone, and there is no cough, we give a further 4 weeks of a different inhaled antibiotic called tobramycin. If there is any cough, we will give 2 weeks of intravenous antibiotics.
Long term inhaled antibiotic treatment
All children who grow Pseudomonas on 3 separate occasions (unless these are separated by several years), need to start long term inhaled antibiotics. This is because we worry that there may be small numbers of Pseudomonas bugs in the lungs that are not completely going away. Long term twice daily inhaled antibiotics help to stop these small numbers of bugs from causing damage. All children with chronic Pseudomonas infection also need to take long term inhaled antibiotics. For both groups of children our first line long term antibiotic is colomycin. For children over 6 years old, this is most conveniently given as Promixin via the ineb nebuliser.
If children on long term colomycin continue to grow Pseudomonas from cough swabs or sputum samples we will switch them over to nebulised tobramycin, initially on its own and the combined with colomycin (taken as one month of colomycin followed by one month of tobramycin), if Pseudomonas infection continues to be a problem.
Aspergillus fumagatus
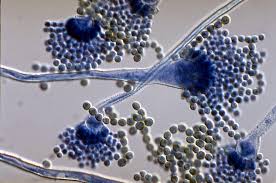 Aspergillus is a very common fungus (mould) found in rotting vegetation, dust and building materials. It releases millions of tiny spores into the air and these are breathed in by everybody everyday. For the vast majority, the spores cause no problems. Rarely they can grow in the mucous of the airways, and even more rarely they can trigger an allergic response called ABPA (see separate section on ABPA). Aspergillus infection can go away on its own without causing any problems, so if children are well, we often do not treat a single positive culture for Aspergillus. If there are symptoms of cough or wheeze or if the Aspergillus is found on multiple airway cultures or if there is ABPA we will treat using an antifungal drug called itraconazole, often for 3 months. Aspergillus is a very common fungus (mould) found in rotting vegetation, dust and building materials. It releases millions of tiny spores into the air and these are breathed in by everybody everyday. For the vast majority, the spores cause no problems. Rarely they can grow in the mucous of the airways, and even more rarely they can trigger an allergic response called ABPA (see separate section on ABPA). Aspergillus infection can go away on its own without causing any problems, so if children are well, we often do not treat a single positive culture for Aspergillus. If there are symptoms of cough or wheeze or if the Aspergillus is found on multiple airway cultures or if there is ABPA we will treat using an antifungal drug called itraconazole, often for 3 months.
Avoiding Aspergillus
To reduce the risk of getting an Aspergillus airway infection, children with CF should avoid rotting vegetation (such as compost heaps and pile of dead leaves), wet straw (such as in a stable - so no 'mucking-out'), building works, grain stores, marshland and bogs.
Difficult to treat infections
There are some bugs that require more complicated treatment - the 3 most common of these are MRSA, Cepacia and NTM. Although infection with these bugs are nearly always acquired from the environment (water, soil, vegetation), it is especially important that these infections do not spread from one child to another within the clinic. This means that anyone who has these infections will need to follow strict segregation rules - see the section on cross-infection.
MRSA
MRSA stands for Meticillin Resistant Staphylococcus aureus. It is exactly the same as normal Staph, but it has become resistant the usual antibiotics used to kill it. This makes it harder to treat, but the bug itself does not do any more damage than the normal Staph bug. MRSA, like any Staph, like to live on the crevices of the skin. When we find MRSA (fortunately we have very few positive cultures for this bug) we try hard to get rid of it, using antibacterial skin cleaners combined with oral antibiotics. If that does not get rid of the infection, we will then use intravenous antibiotics. The protocol we follow can found on the Health Professionals section of the website.
Cepacia
Cepacia (ke-pay-shah) is a bacterial bug a bit like Pseudomonas. It can cause permanent airway infection which cannot be cleared with antibiotics. Cepacia has 10 variants from a family of bacteria called Burkholderia. Some are worse than others. They are all resistant to many antibiotics and hard to treat. B. cenocepacia is probably the worst of the bunch and occasionally can cause rapidly worsening lung disease. Treatment is with combinations of intravenous and nebulised antibiotics (see the Cepacia tab on the Health Professionals section of the website for more details).
NTM
Non-tuberculous mycobacteria (NTM) are naturally resistant to antibiotics and hard to treat. There are a variety of different types of NTM, the most troublesome is which is M. abscessus. Infection with NTM is associated with an increase the rate of decline in lung function and every effort must be made to clear NTM infection when it is found. All treatment takes a long time - usually 12 to 18 months of therapy. For some types of NTM this can be using a combination of 3 or more oral antibiotics. For M. abscessus the treatment is more difficult, and involves an initial 4 week course of intravenous antibiotics and then a combination of 3 oral antibiotics and 2 nebulised antibiotics plus more iv antibiotics every 3 months. This is a very big deal for any child and family. To be sure it is necessary, NTM infection is only confirmed if it is found on 3 sputum samples, or if children cannot cough up sputum, then on a single bronchoscopy sample. Treatment of M. absecssus seems to be successful in clearing the infection in about 60% of children, and keeps it under control in the remainder. See the NTM tab on the Health Professionals section of the website for more details of treatment for NTM.
| 




